BLOG • Feb 19, 2025
Unlocking Revenue Potential: Why CARC Codes Are Essential for Denial Management
Dedicated to Delivering High-Quality Risk Adjustment Coding
Schedule a CallIn DNFB
Clinical validation denials
Audit-grade DRG/APC Accuracy
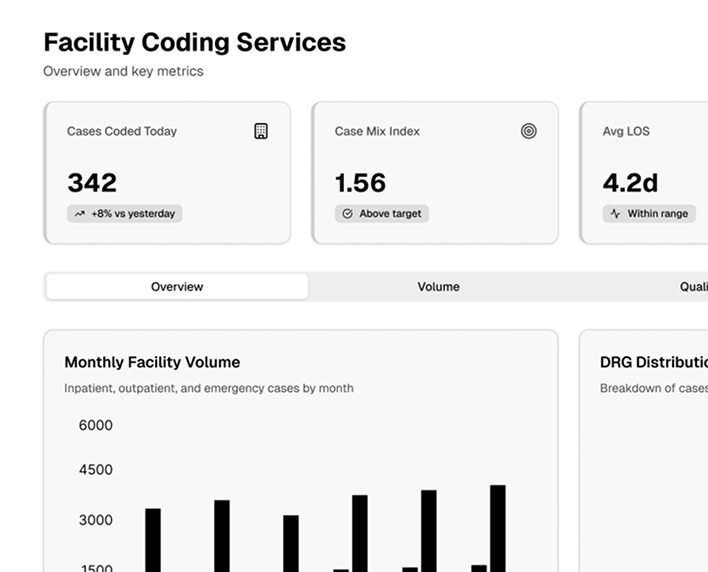
From inpatient to outpatient environments, our certified coders and advanced tools ensure your claims are processed accurately and on time.
Our experts are equipped to handle diverse coding needs across inpatient, outpatient, and emergency settings. We deliver consistent accuracy—even during peak volumes.
Our processes are designed to minimize errors, align with current coding regulations, and ensure high-quality output across all operations.
We provide actionable insights, including CDI assessments, MS-DRG vs. APR-DRG comparisons, and GM-LOS vs. actual LOS analyses.
Our coders can be integrated flexibly into your team to maintain productivity and continuity during high-volume or transition periods.
Our meticulous coding reduces costly denials and ensures full reimbursement through proactive documentation and compliance strategies.
Our facility coding operations are designed to deliver precision, compliance, and scalability, ensuring seamless integration with your facility’s workflows
Our operations integrate AI-enhanced CDI tools to identify documentation gaps and ensure alignment with coding requirements. These tools help reduce ambiguities, strengthen documentation accuracy, and maximize reimbursement potential
We provide specialized coding expertise across various facility environments, including inpatient admissions, surgical units, emergency departments, outpatient services, urgent care centers, and ancillary departments like radiology and pathology
Our advanced rules engine cross-verifies codes against current payer-specific policies, regulatory standards, and coding guidelines. This ensures accurate code assignment and compliance with ICD-10, CPT, HCPCS, and MS-DRG requirements
Our customizable workflow tools optimize coder productivity by streamlining task allocation, prioritizing urgent cases, and providing built-in coding references. This reduces turnaround times while maintaining accuracy and complianc
Seamlessly integrate coding operations with your RCM platform to enable end-to-end visibility of claims, reduce revenue leakage, and expedite the billing process. Our solutions align coding with billing to ensure smoother claim submissions

Our operations include predictive analytics to assess patterns in denials, identify root causes, and implement preventive measures. This proactive approach minimizes rejected claims and enhances overall financial performance
Utilize our secure remote coding infrastructure to manage workloads across multiple facilities or during staffing shortages. Our HIPAA-compliant cloud-based systems ensure data security while providing operational flexibility
Access detailed reports tailored to your facility’s needs, including coding productivity, quality metrics, clinical documentation improvement trends, and reimbursement analysis. These insights empower data-driven decision-making for continuous improvemen
Our coders and compliance teams are equipped to perform targeted or full-scale coding audits, ensuring adherence to payer and regulatory requirements. These audits help identify gaps, rectify errors, and improve long-term compliance strategies
We provide training sessions and documentation reviews to upskill your in-house teams. This includes workshops on the latest coding updates, regulatory changes, and payer-specific coding nuances to enhance overall operational excellence