BLOG • Feb 19, 2025
Unlocking Revenue Potential: Why CARC Codes Are Essential for Denial Management
Stop denials before they happen. Our proactive approach optimizes revenue, reduces rework, and ensures a smoother billing experience
Schedule a CallClaim Denial Rate
Denial Appeal Success Rate
Average Denial Resolution Time


Healthcare organizations can significantly improve their cash flow, reduce revenue leakage, and maintain positive patient experiences by leveraging accurate coding, efficient follow-up protocols, and strategic payer negotiation.
Through thorough root-cause analysis, healthcare providers can develop targeted strategies to prevent recurring issues. Key initiatives include reviewing claim forms for missing or mismatched data, verifying patient eligibility and coverage details, and conducting internal audits to identify coding inconsistencies.
Transparent communication between providers and payers is crucial for effective denial management. Clear contact channels and standardized appeal procedures accelerate resolution, while timely follow-ups, direct escalation pathways, and data-driven dialogue help reduce future denials.
Real-time claims tracking, EHR systems, and analytics tools assist healthcare facilities in swiftly identifying denials. Incorporating these solutions into billing workflows allows for denial monitoring by category, automated resubmissions, and thorough performance reporting to detect trends.
Team competency is crucial for preventing denials. Ongoing training on payer rules, coding updates, and regulatory requirements ensures claims are submitted correctly. Key steps include continuous education on policies, cross-department collaboration for compliance, and frequent refresher courses to stay ahead of industry changes.
Beyond operational and technical efforts, a successful patient financial services strategy emphasizes patient engagement and satisfaction. Improving transparency about patient responsibility and simplifying billing processes helps minimize confusion, build trust, and ultimately enhance patient retention and satisfaction.
A successful denial management operation requires a structured workflow that begins with accurate claim preparation and ends with actionable insights for continuous improvement.
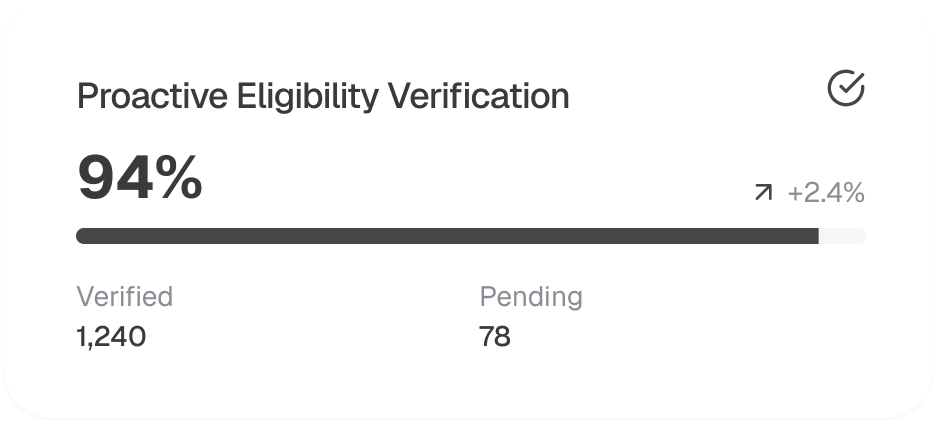
Accurate coverage details from the start significantly decrease denials. Common tactics include real-time eligibility checks before visits, collecting and verifying insurance information at registration, and confirming authorization requirements for specialist services.
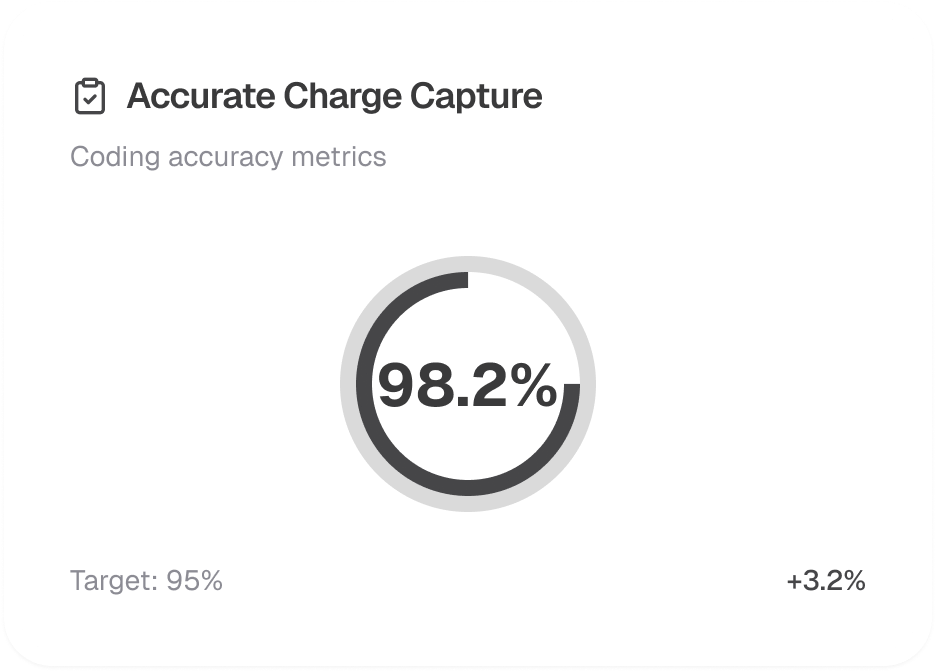
Accurate coding minimizes denials and optimizes reimbursements. Employing certified coders and using current code references ensures correct mapping of clinical documentation, reduces billing discrepancies, and aligns with payer-specific guidelines.
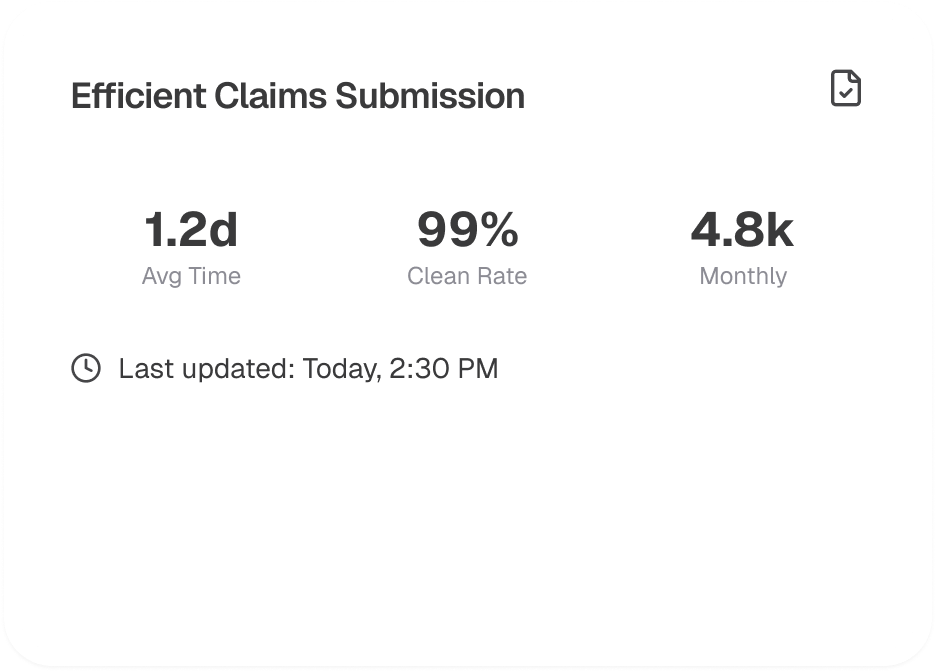
A pre-submission scrubbing process helps detect errors leading to denials. This involves using claim-editing software to spot missing modifiers or mismatched data, verifying accuracy against payer rules, and flagging potential underpayments for review.
Swift action on denials is essential. A structured protocol involves categorizing denials by type, prioritizing high-value claims for immediate appeal, and compiling all necessary clinical documentation and justification.
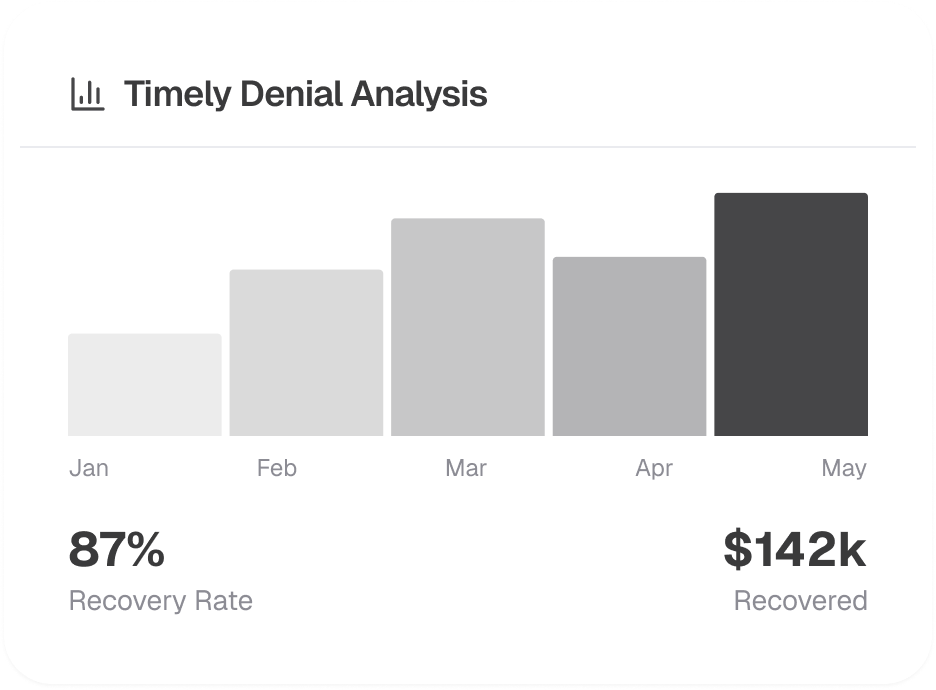
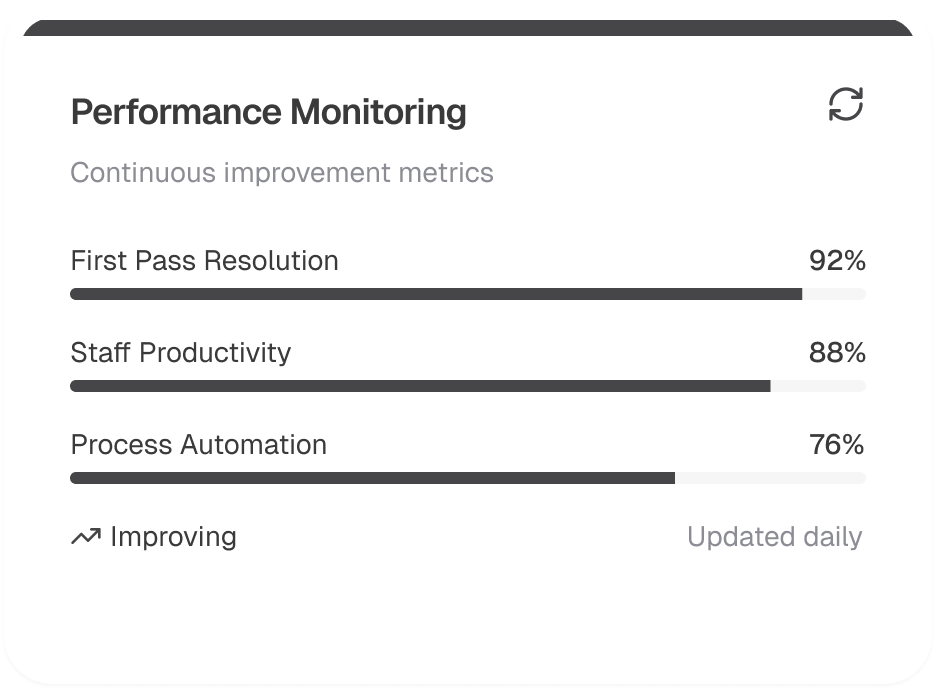
Ongoing analysis of denial trends and root causes fosters lasting improvements. By monitoring KPIs like Denial Rate, Days in A/R, and Appeal Success Rate, organizations can pinpoint workflow enhancements, implement targeted process changes, and cultivate a culture of accountability and proactive revenue cycle management.