BLOG • Feb 19, 2025
Unlocking Revenue Potential: Why CARC Codes Are Essential for Denial Management
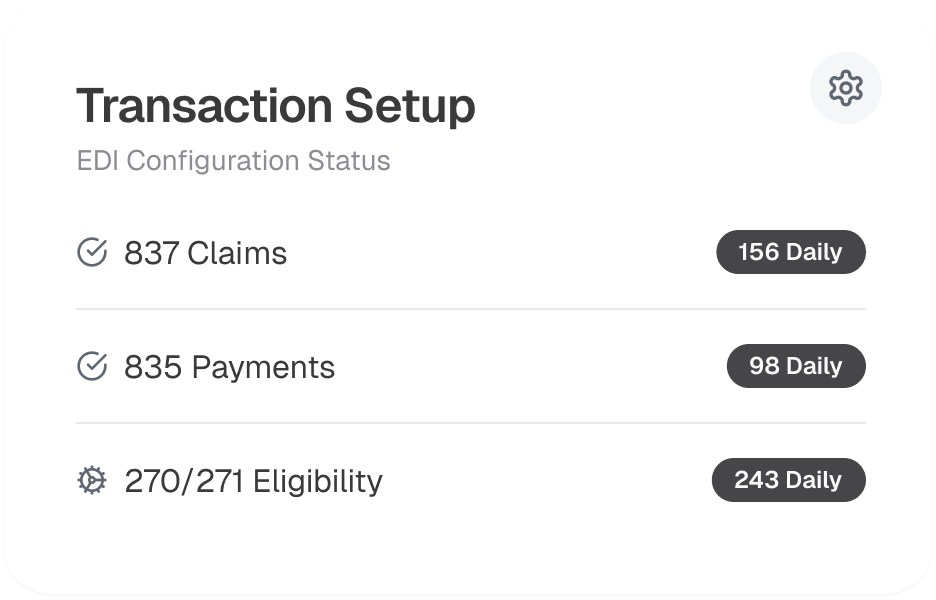
Breeze through EDI. Enjoy faster, more secure transactions so you can keep your focus on patient care
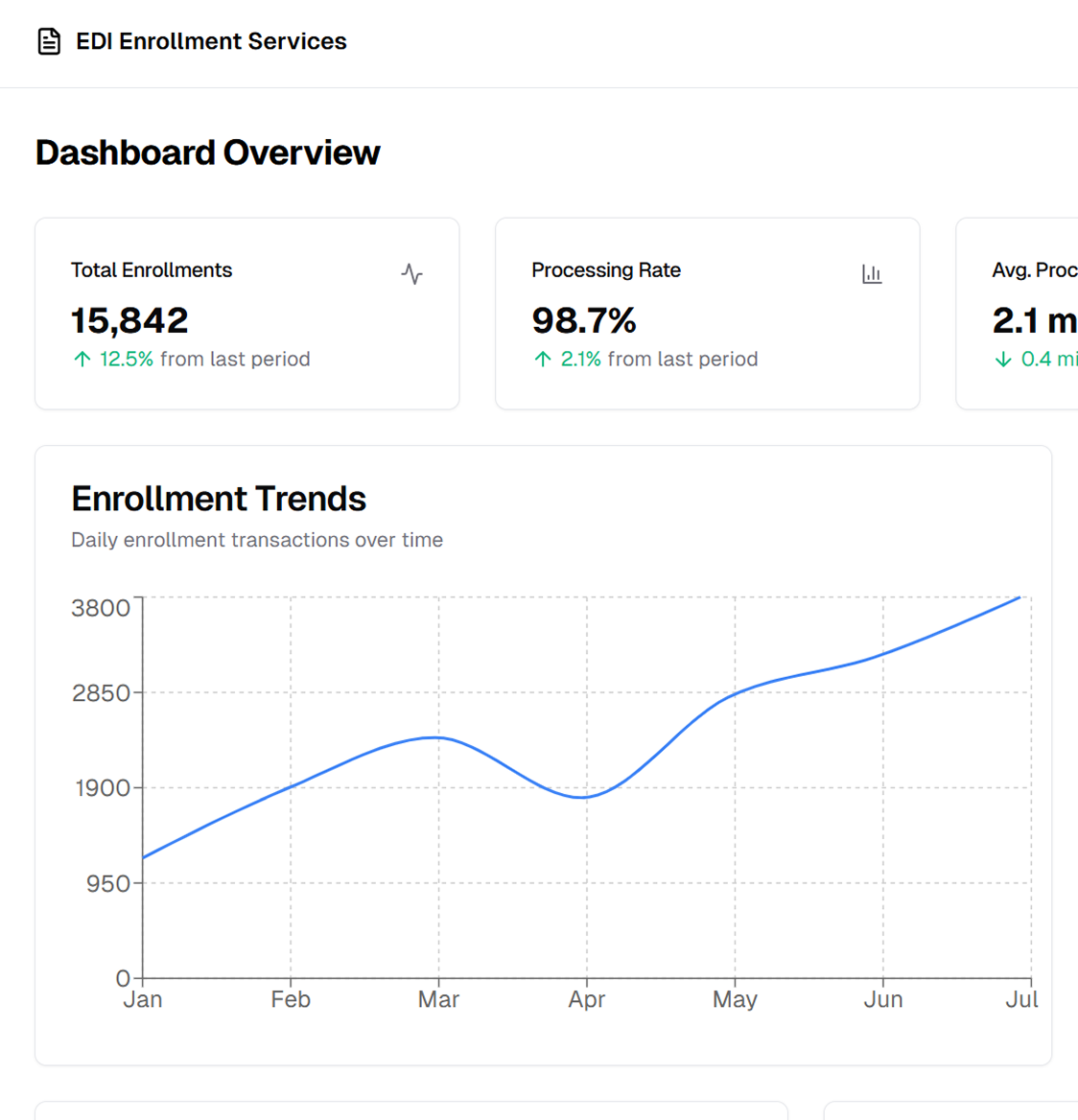
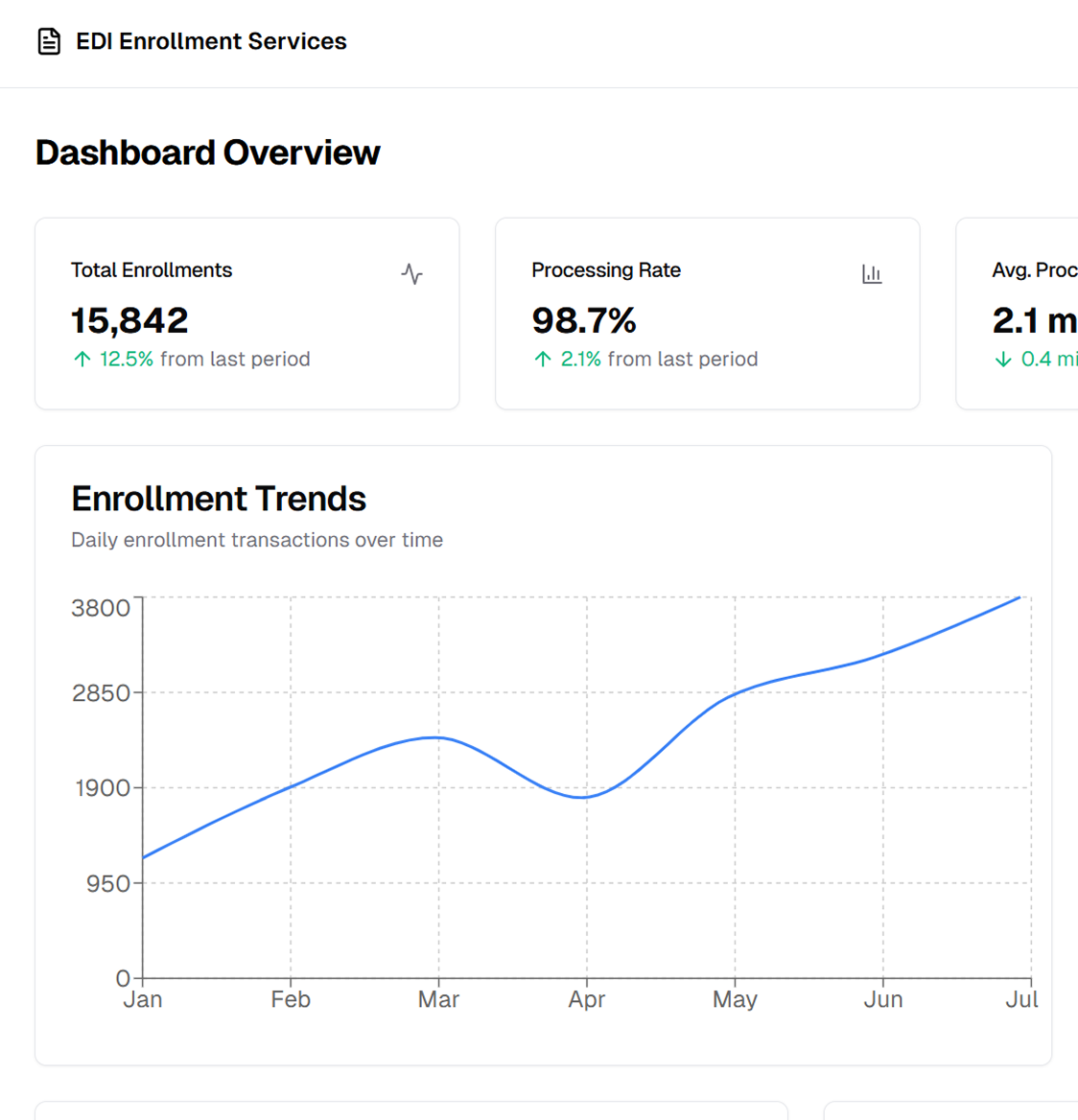
Schedule a CallSuccessful EDI Enrollment Rate
Average Enrollment Processing Time
Enrollment Rejection Rate
Our EDI Enrollment Services manage the entire process, from credentialing and documentation to testing and activation, ensuring uninterrupted electronic transactions that improve revenue cycle efficiency and reduce administrative burdens
EDI enrollment enables providers to securely transact with payers and clearinghouses, reducing manual work, claim denials, and reimbursement delays. A structured process ensures accurate setup, compliance, and efficient revenue cycle management
Not meeting these can lead to processing delays and claim rejections. Our team ensures compliance with guidelines, submits forms and manages approvals for Medicare, Medicaid, commercial insurers, and third-party administrators. We ensure all transactions comply with payer protocols and HIPAA standards, streamlining processes and reducing administrative burdens to eliminate enrollment delays
Claim status inquiries allow tracking of submitted claims without manual follow-ups, while referral requests simplify prior approvals for services. Properly configured transactions result in smooth operations and quicker claims adjudication
We handle the technical setup and integration of EDI transactions within EHR, practice management, and revenue cycle platforms, enabling seamless electronic transactions without manual intervention, reducing processing time, and improving claim acceptance rates
Once certified, we facilitate transaction activation and monitoring for uninterrupted processing. By managing the end-to-end testing and activation, we reduce claim rejection risks due to incorrect EDI configurations, helping providers achieve efficient electronic transactions
Our EDI Enrollment Services cover every process stage, from payer credentialing and registration to real-time transaction monitoring and ongoing compliance management
The first step in EDI enrollment is provider credentialing and payer registration. We handle all necessary documentation. We manage electronic fund transfer (EFT) and electronic remittance advice (ERA) enrollment, enabling providers to receive automated payments and remittance details

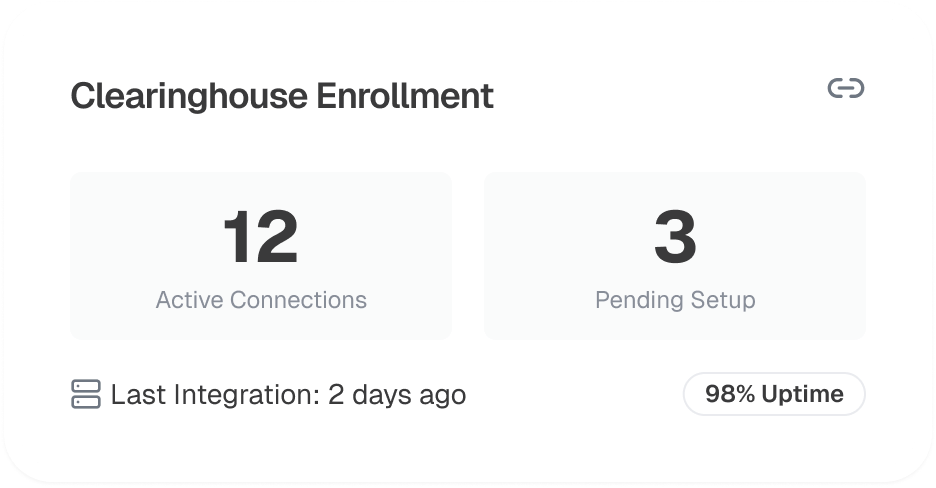
To facilitate EDI transactions, providers must enroll with clearinghouses that act as intermediaries between them and payers. We manage the selection and setup of clearinghouses based on payer network compatibility and provider requirements, ensuring seamless data exchange
An EDI system is crucial for error-free claims processing and payment reconciliation. Our team sets up all transaction types in the provider’s EHR or revenue cycle platform, including claim submissions, electronic remittances, and eligibility verification. We also validate payer-specific EDI formats to avoid claim rejections and ensure smooth processing
Before an EDI transaction activates, it undergoes testing to ensure accuracy and compliance. We handle test file submissions to payers and clearinghouses, identifying and correcting formatting or compliance errors to prevent claim rejections

EDI enrollment requires ongoing updates to ensure smooth operations. Our team handles payer enrollment updates, keeping providers compliant with changing requirements. Regular performance audits optimize EDI workflows and improve processing efficiency