BLOG • Feb 19, 2025
Unlocking Revenue Potential: Why CARC Codes Are Essential for Denial Management
Get ready for healthcare's future. Ensure your credentials are current, valid, and up to the challenge
Schedule a CallFirst-pass approvals
First In-Network Claim
On-time renewals
Partnering with a dedicated credentialing service ensures healthcare professionals meet requirements, maintain privileges, and participate in insurance networks, reducing administrative burdens, complying with standards, and protecting revenue streams
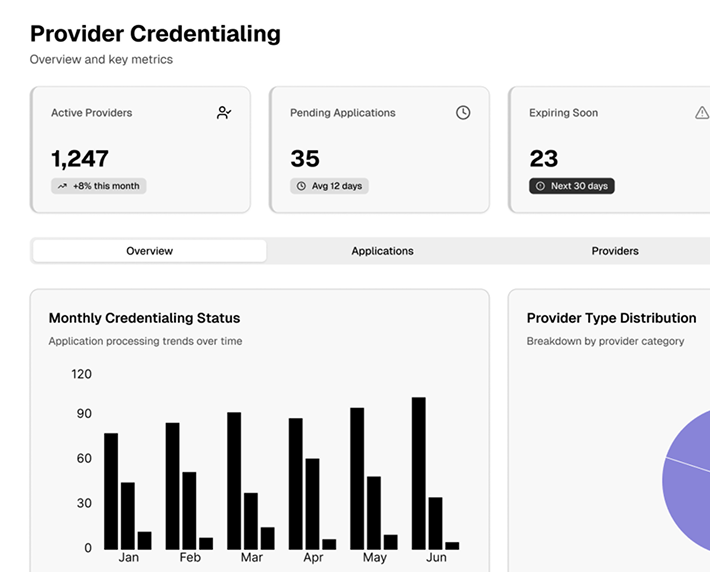
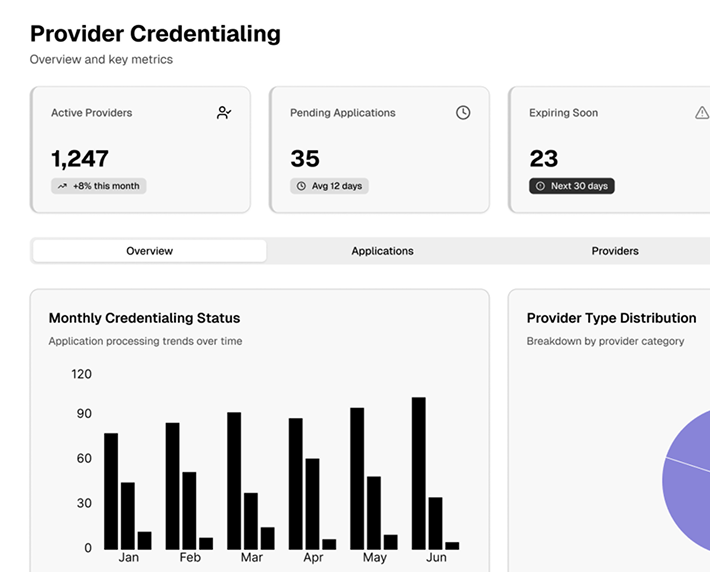
• Efficient Documentation: We take the chaos out of credentialing paperwork by systematically organizing, reviewing, and compiling essential forms. • Automation Integration: Leveraging automated solutions (e.g., Electronic Data Interchange (EDI), Electronic Remittance Advice (ERA), Electronic Fund Transfer (EFT)) to minimize errors and expedite submissions. • Industry-Leading Turnaround: Our average credentialing timeline is 90–100 days—one of the fastest in the industry
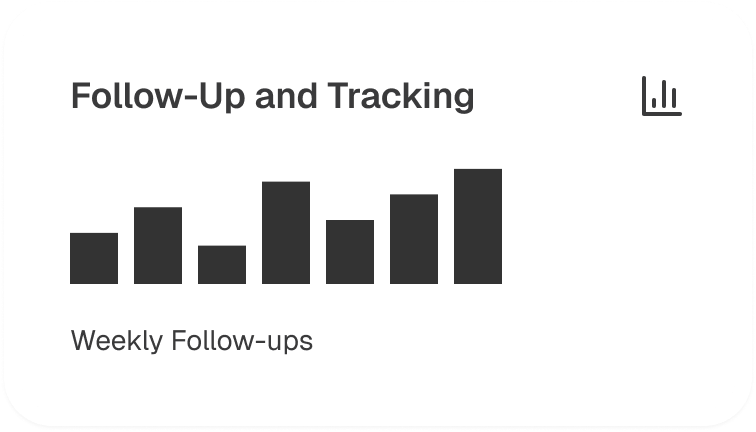
• Proactive Tracking: Our team closely monitors every step of your application, ensuring no missed deadlines or requests. • Regular Status Updates: Stay informed with periodic progress reports on your enrollment, licensing, and certification milestones. • Payer Relationship Management: We communicate directly with insurance carriers to confirm receipt of applications and clarify any requirements
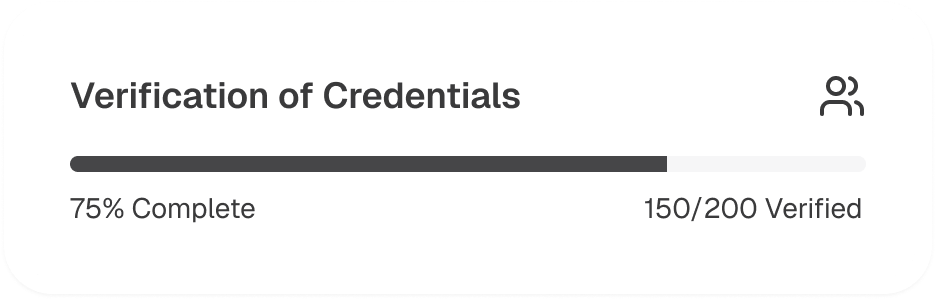
• Primary Source Verification: We verify essential credentials—DEA registrations, State Medical Licenses, Board Certifications—directly from the originating authorities • Professional Background Checks: Employment history verification, malpractice checks, and reference reviews assure complete compliance • Universal Checklist Implementation: A standardized checklist for every provider ensures no detail is overlooked, optimizing efficiency
• Medicare/Medicaid Applications: We use PECOS, CMS Forms, and state portals for correct and timely enrollments • Managed Care Organizations (MCOs): Seamlessly integrate providers with commercial payers for improved patient access and expanded service coverage • CAQH Maintenance: Continuous updates of provider data in CAQH to streamline future enrollments and re-credentialing processes
• Collects background details via an email-based questionnaire for accurate credentialing • Our team reviews applications and communicates with payers, licensing boards, and institutions • Finalizes enrollment and supports revalidation and re-credentialing for compliance
Our credentialing operations, backed by a dedicated team, advanced automation tools, and a proven follow-up system, ensure compliance standards are consistently met from data gathering to contract finalization
• Form Completion: We handle all paperwork required by payers, government programs, and licensing bodies. • Technical Documentation: Ensuring EDI, ERA, and EFT enrollments are accurately processed for efficient financial transactions. • Document Management: Maintain, store, and securely share vital records throughout the credentialing lifecycle
• Primary Source Verification: Validate each provider’s education, training, licenses, and certifications. • Employment History Checks: Confirm professional background to bolster credibility and compliance. • Compliance with Standards: Follow all state-specific and federal guidelines (e.g., NPPEs checks, DEA validations)
• Real-Time Updates: Frequent status reports to providers on submitted applications • Payer Liaison: Direct interaction with carriers to confirm receipt and accelerate approvals • Issue Resolution: Address any application discrepancies, requests for additional documentation, or clarifications immediately
• Regular Renewals: Proactively manage license renewals, DEA registrations, board certifications, and malpractice coverage • Data Updates: Maintain CAQH profiles and provider databases to meet evolving payer standards • Continuous Compliance: Ensure up-to-date submissions and verifications to prevent lapses in coverage or network participation
• Fee Schedule Analysis: Scrutinize payer proposals, compare against market benchmarks, and guide providers in negotiating optimal terms • Financial Well-Being: Maximize reimbursement rates and secure favorable contract clauses • Network Optimization: Expand or refine in-network participation to enhance revenue and patient access

• Source Validation & Quality Checks: Constantly verify practitioner and facility details for accuracy • Technical Support: Assist in obtaining missing documents, updating payer databases, and troubleshooting enrollment platforms • Scalable Services: Adapt credentialing support to your practice’s growth, integrating new providers swiftly