BLOG • Feb 19, 2025
Unlocking Revenue Potential: Why CARC Codes Are Essential for Denial Management
Learn how to maintain a hassle-free process for both self-pay and patient invoices, ensuring timely payments and satisfied patients
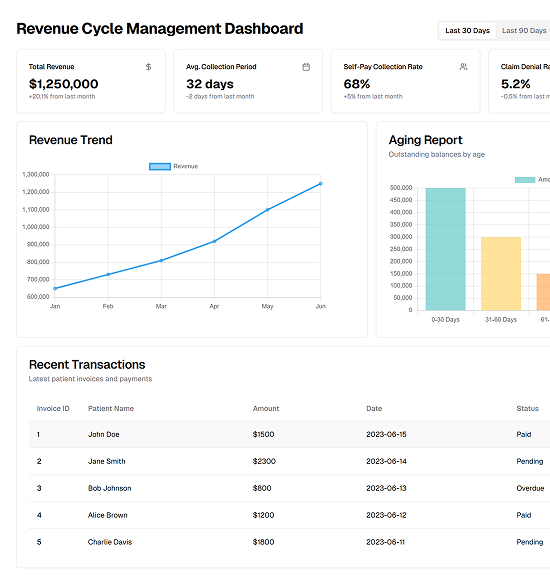
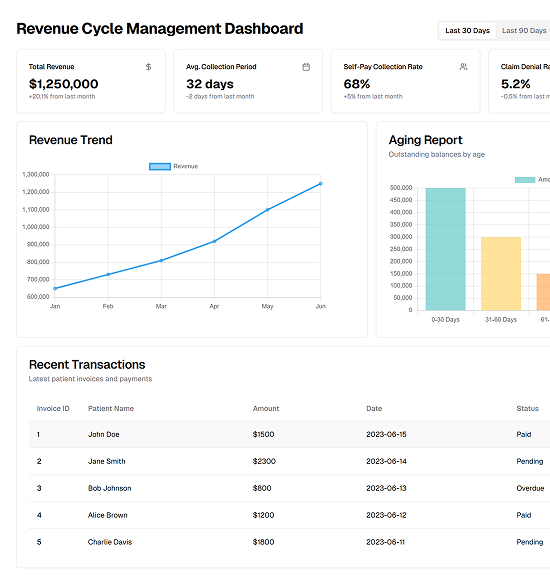
Schedule a CallAverage Days to Payment
Self-Pay Collection Rate
Patient Invoice Outstanding Balance
We take a data-driven approach to eligibility verification that prioritizes efficiency, accuracy, and compliance. Here’s why healthcare providers and patients trust us
Every invoice should include the patient’s full name, date of birth, and contact details to ensure accurate identification
Communicate financial policies and provide cost estimates to patients before their appointments. This proactive approach sets clear expectations and reduces post-service billing disputes
Provide a detailed breakdown of all services rendered, including procedure or CPT codes, descriptions, and associated charges
Craft invoices that are clear, concise, and free of technical jargon. A clean layout with contact details for billing questions makes it easier for patients to engage with the process
After issuing the invoice, implement structured follow-ups for unpaid bills. Use a combination of reminder letters, emails, and phone calls to keep patients informed and encourage timely payments
Managing self-pay collections effectively requires a patient-centered approach that prioritizes transparency, flexibility, and compliance
Effective communication with patients ensures transparency and builds trust. Pre-visit notifications, clear invoicing, and proactive follow-ups help patients understand their financial obligations and reduce disputes

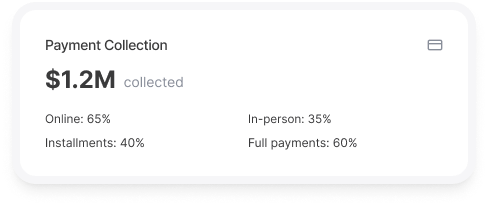
Streamlining payment collection processes, such as upfront co-pays and offering flexible payment plans, minimizes outstanding balances. Providing multiple payment options ensures convenience for patients
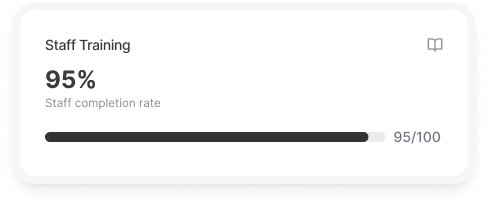
Equipping staff with billing and compliance knowledge enhances patient interactions and operational efficiency. Workflow automation tools reduce manual effort and improve productivity
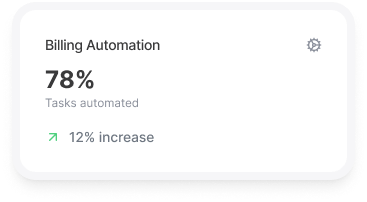
Automated billing systems integrated with Electronic Health Records (EHR) streamline invoice generation, payment tracking, and account management, reducing errors and saving time
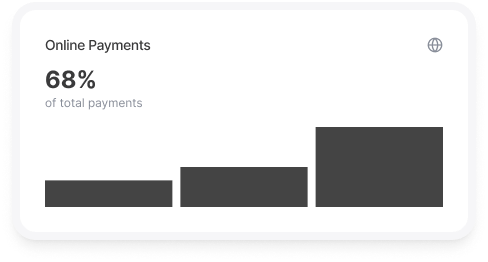
User-friendly, secure portals allow patients to view invoices, make payments, and set up plans conveniently. Mobile compatibility enhances accessibility and usability
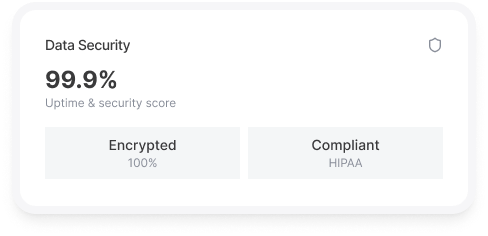
Ensuring HIPAA compliance through encryption, restricted access, and secure data handling protects sensitive patient and financial information from breaches
Analytics tools provide insights into payment trends, account receivables, and performance metrics, helping to optimize collections and financial forecasting
Integrated systems enable seamless insurance verification, accurate cost estimation, and efficient data sharing with third-party collection agencies when needed
Strict adherence to regulations like HIPAA and the Fair Debt Collection Practices Act (FDCPA) is essential to protect patient rights and maintain ethical billing practices. Accurate documentation further ensures accountability